Urinary Incontinence in Women

Urinary Incontinence in Women
- Urinary Incontinence in Women
- Urinary Incontinence in Older Adults
- Diagnosis of Urinary Incontinence
- Treatment for Urinary Incontinence
- Managing Urinary Incontinence
- For More Information on Urinary Incontinence
- Urinary Incontinence | Treatments, Causes, Types And Symptoms
- URINARY INCONTINENCE Overview
- STRESS URINARY INCONTINENCE
- Male Stress Urinary Incontinence
- Female Stress Urinary Incontinence
- How can you prevent urinary incontinence?
- Tips For Dealing With Urinary Incontinence
- Urinary Incontinence in Men
- Urinary incontinence (UI) introduction
- Urinary Incontinence Causes and Treatment
- Urinary incontinence (UI) in men facts
- What causes urinary incontinence (UI) in men?
- How is urinary incontinence (UI) in men diagnosed?
- How is urinary incontinence (UI) in men treated?
- What medications relieve pain and treat urinary incontinence in men?
- Resources for urinary incontinence in men
- Top Urinary Incontinence Related Articles
- Know Your Risk Factor for Urinary Incontinence
- What Causes Urinary Incontinence?
- What Are the Treatments for Urinary Incontinence?
- Types of Urinary Incontinence & Their Treatment
- Living With Urinary Incontinence? Don't Let It Be Your Secret
- Urinary Incontinence - Types And Causes And Products
- 3.6.1.5 Urinary Incontinence
- What types of urinary incontinence exist?
- Find Urinary Incontinence Care Near You
- Relieve Yourself of Urinary Incontinence in Des Moines
- Transient Urinary Incontinence
- Chronic Urinary Incontinence
Urinary Incontinence in Women
Compared with baseline, women in the treatment group had significant. Improvement in urinary frequency (14 percent reduction), and proportion. Of voids associated with urgency (30 percent reduction). 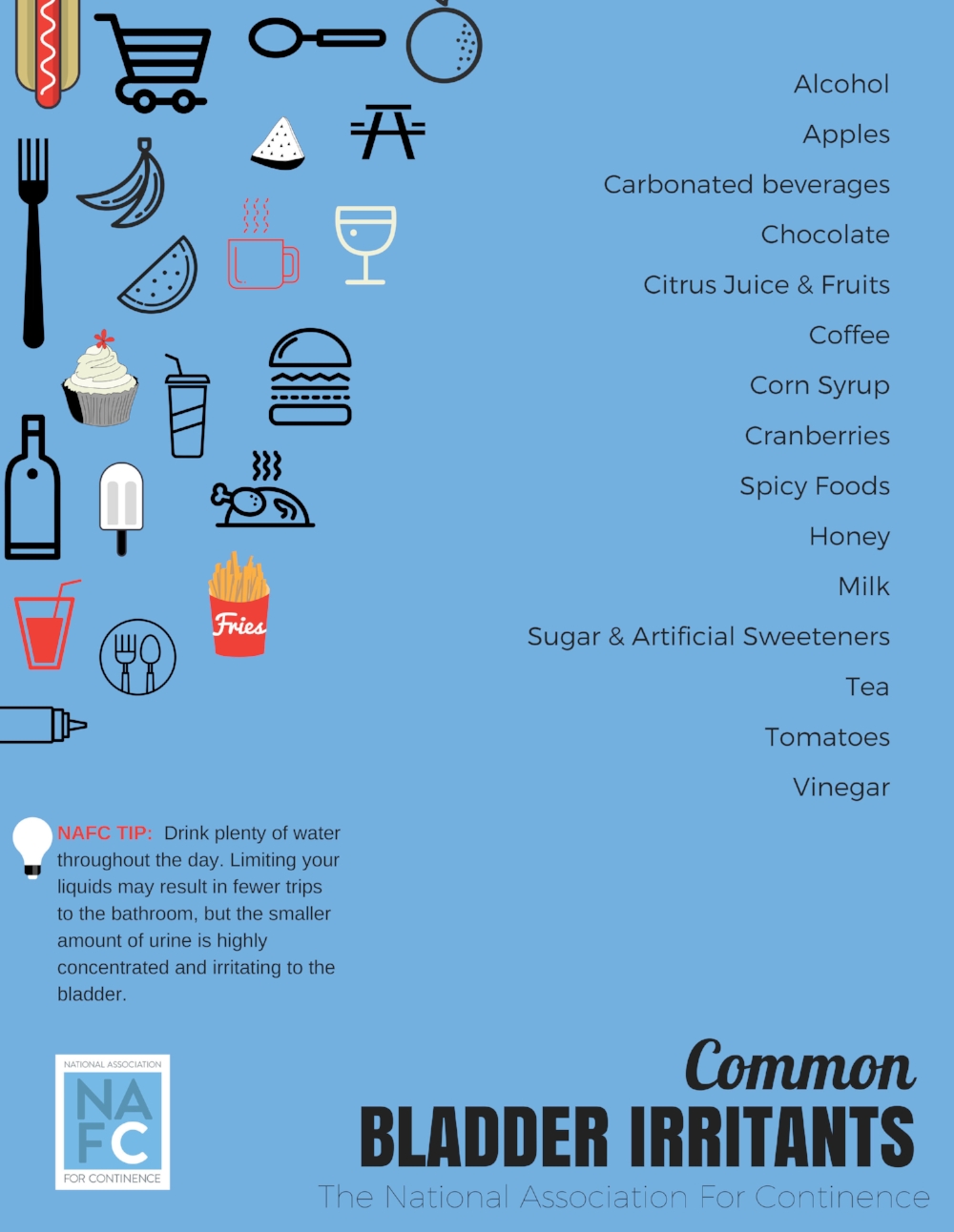
Usually, it is asymptomatic and gets discovered during clinical examination or imaging. Some women experience uterine bleeding, urinary frequency, and pelvic pain.
Both men and women can have incontinence during and after surgery or some other treatments for cancer. Incontinence can also occur because of other non-cancer medical conditions.
Urinary Incontinence in Older Adults
“urinary incontinence (ui) is a natural way of life. Most older adults have this problem, and they can't do much about it. 
Older dogs (especially spayed females, may be prone to urinary incontinence, where their bladder sphincter tone becomes weakened, due to estrogen levels which drop after spaying.
Other, less common types of incontinence include:. Functional incontinence: older adults or disabled people may experience incontinence simply because a physical or mental impairment keeps them from making it to the toilet in time.
Diagnosis of Urinary Incontinence
Infections are decreased, saving staff time and lowering disposables costs for the facility. The bladderscan instrument aids in the diagnosis, management and treatment of urinary outflow dysfunction. 
Do you cross your legs when you feel a sneeze coming on? do sudden urges to go cause you to panic? do leaks just happen randomly, without notice? these are all symptoms of a condition known as urinary incontinence, or ui.
Women can have both urinary and bowel incontinence. Below are different types of bladder incontinence. Types of incontinence. Mirabegron (betmiga™) – may also increase bladder capacity.
Treatment for Urinary Incontinence
A full diagnostic evaluation of urinary incontinence requires a medical history, physical examination, urinalysis, assessment of quality of life and, when initial treatments fail, invasive urodynamics.
Fortunately, there’s plenty a woman can do to rein in urinary incontinence, and most solutions don’t require medication. In fact, new guidelines on urinary incontinence from the american college of physicians urge doctors to recommend pill-free treatments first.
If you experience urinary incontinence, tell your doctor. He or she can provide basic treatments for urinary incontinence. For more persistent symptoms, your doctor may refer you to specialist with expertise in evaluating and treating urinary incontinence.
Managing Urinary Incontinence
This quality standard covers managing urinary incontinence in women (aged 18 and over). It covers assessment, care and treatment options.
Diagram of an intermittent catheter in place in a male for clean intermittent catheterization (cic). There are three types of catheter products that are used for managing urinary incontinence: indwelling (sometimes called a foley) catheters, suprapubic catheters, and intermittent catheters.
Homeopathic remedies for women. Once you address these two issues, there are also several homeopathic remedies available, depending on the type of urinary incontinence that you are managing:.
For More Information on Urinary Incontinence
Urinary Incontinence in Women
This information can help the doctor pinpoint the type of ui you have. Male urinary incontinence treatment can involve a number of different approaches.
". "treatments for urinary incontinence in women. " national. Kidney and urologic diseases information clearinghouse. National. Institute of diabetes and digestive and kidney diseases.
Patient information. Clinician information. Urinary incontinence (ui) is the loss of control of urine, or the inability to hold urine in until a bathroom can be reached.
Urinary Incontinence | Treatments, Causes, Types And Symptoms
There are different types of urinary incontinence and to know the causes, symptoms and treatments of urinary incontinence, read the following articles.
URINARY INCONTINENCE Overview
In: kim ed. Urinary incontinence. New york, ny: webmd. Http://emedicine. Medscape. Com/article/452289-overview. Updated november 28, 2016.
Surgery overview�. If a person is suffering from stress urinary incontinence or overactive bladder, the permanent solution is to undergo surgery, making living easier and bringing full stop to your problem.
Overview of stress urinary incontinence. Urinary incontinence (ui) is defined by the international continence society (ics) as “the complaint of involuntary leakage of urine.
STRESS URINARY INCONTINENCE
Stress urinary incontinence (sui) is the most common form of urinary incontinence in women and is associated with high financial, social, and emotional costs.
Urinary incontinence is the involuntary excretion of urine from one's body. Stress incontinence is essentially due to pelvic floor muscle weakness.
Mixed incontinence – a combination of stress and urge incontinence. Many tests are available to help diagnose the different forms of urinary incontinence, with the most common being a pelvic exam.
Male Stress Urinary Incontinence
There are five different types of urinary incontinence, as outlined below. Stress incontinence occurs when there is a leakage of urine due to pressure on your abdomen, like when coughing, laughing or lifting something heavy.
It can also be due to medications. Women especially elderly ones can suffer from mixed urinary incontinence and the most common being the urge and stress urinary incontinence.
Urinary incontinence falls into six categories: stress incontinence, urge incontinence, incontinence without sensory awareness, overflow incontinence, mixed incontinence, and functional incontinence.
Female Stress Urinary Incontinence
History. Continuous urinary incontinence (cui) is the complaint of continuous leakage (2). Uncategorised incontinence: is the observation of involuntary leakage that cannot be classified into one of the categories (stress or urgency incontinence) on the basis of signs and symptoms (2).
Study population: adult women with stress urinary incontinence (ui), urge ui, or mixed ui. Efficacy end points: patient-perceived cure or improvement, symptoms, quality of life, frequency of leakage episodes, amount of urine lost.
Bladder leaks, urinary incontinence, or stress incontinence, is the involuntary leaking of urine when coughing, straining or exercising. The pessary works by applying pressure onto the urethra (which drains the bladder) against the pubic bone and lifts the lower part of the bladder.
How can you prevent urinary incontinence?
2010;29(1):4-20. Doi: 10. 1002/nau. 20798. Pmid: 19941278. Shamliyan t, wyman j, bliss dz, et al. Prevention of urinary and fecal incontinence in adults.
Concepts. 207170000, 207174009, 41840003, 158469002, 139399005, 142633003, 158472009, 236661008, 165232002. Lnc. La6436-5. English. Incontinence, urinary, bladder incontinence, micturition involuntary, urinary incontinence, urination involuntary, urine incontinence, unable prevent bladder emptyng, incontinence of urine nos, [d]incontinence of urine (context-dependent category), [d]incontinence of urine nos (context-dependent category), unspecified urinary incontinence, urine incontinence, [d]incontinence of urine, [d]incontinence of urine nos, unable to restrain urination, loss of control of urination (symptom), incontinent of urine, urinary loss of control, unable to restrain urination (symptom), loss of control of urination, urinary incontinence, urinary incontinence (diagnosis), incontinence urinary, micturition involuntary, urination involuntary, urinary incontinence nos, urinary incontinence [disease/finding], bladder incontinent, urine incontinent, leaking urine, unable (to);hold urine, incontinence;urine, urination;involuntary, incontinent bladder, urinary incontinences, urine incontinence, bladder incontinence, loss of bladder control, bladder control loss, urine leak, urine leaking, weak bladder, [d]incontinence of urine (situation), bladder: incontinent (finding), [d]incontinence of urine nos (situation), bladder incontinence, incontinence of urine, absence of bladder continence, urinary incontinence, involuntary urination, lack of bladder control, leaking of urine, loss of bladder control, ui - urinary incontinence, unable to control bladder, unable to hold fluids, unable to hold urine, unable to prevent bladder emptying, weak bladder, bladder: incontinent, urine incontinence, urinary incontinence (finding), incontinence urine, bladder; weak, incontinence; urinary, urine; incontinence, weak; bladder, incontinence (urinary), urinary incontinence, urinary incontinence, unspecified, involuntary urination, unable to hold urine.
In summary, the mechanism by which pueraria mirifica has been found to improve female urinary function and reduces incidences of urinary incontinence and urgency in post menopausal women is by strengthening and improving the functioning of the muscles of the urethral sphincter and other smooth muscle urethra tissues and pelvic floor muscles, thus preventing uncontrolled urination in response to a bladder spasm or from various stresses on the bladder.
Tips For Dealing With Urinary Incontinence
Strategies for dealing with nighttime incontinence. There are several ways to head off nighttime urinary incontinence. Try the following tips:.
How can you get rid of urinary incontinence?. For most people, some self-help tips and lifestyle changes are sufficient to get relief, and these include:.
When the urologist is dealing with a frail elderly patient with urinary incontinence, collaboration with other healthcare professionals such as elderly care physicians is recommended.
Urinary Incontinence in Men
Options that in some cases can offer better protection thereby making the child feel more comfortable and secure. I've talked with customer service reps from the bedwetting store,continence connection,and hdis and other places that sell incontinence products and the ones i spoke with felt that the disposable briefs tend to be more absorbent and provide better protection than garments such as pull-ups and "goodnites" although some people i've spoken with said that both briefs and pull-ups are equally effective at protecting the user,it's just a question of personal preference.
Urine loss during activities such as coughing, sneezing, laughing, jumping, or lifting. Pregnancy, childbirth, menopause, pelvic radiation, surgical trauma. Urge. An occasional sudden need to urinate with large volume urine loss; can also exist without incontinence.
More than 13 million people in the united states -- male and female, young. And old -- experience incontinence. Women experience incontinence twice as.
Urinary incontinence (UI) introduction
Apples and apple juice. Many medications can contribute to urinary incontinence, according to harvard health , including:. Diuretics, such as lasix (furosemide) and bumex (bumetanide), which increase the production of urine by the kidneys.
Urinary incontinence (ui) causes accidental leakage of urine. It isn’t a disease, but rather a symptom of another condition. This underlying medical issue causes a loss of bladder control.
Metoclopramide can cause side effects that include headache, drowsiness, fatigue, sleep problems, diarrhea, dizziness, constipation, and dry mouth. Contact a medical professional if you experience mood changes, restlessness, suicidal thoughts, urinary incontinence, and discharge from the nipples.
Urinary Incontinence Causes and Treatment
For more information on treatment and management of urinary incontinence, visit urinary incontinence in older adults. Because most urinary tract infections are caused by bacteria, bacteria-fighting medications called antibiotics are the usual treatment for utis.
These treatments should bring relief to most people who have urinary incontinence. However, if the treatments do not work for you, many absorbent protective pads are available to use.
Urinary incontinence (ui) is common among women and contributes to decreased quality of life. Several effective treatment options are available for the most common types of ui (stress, urge, and mixed), including lifestyle and behavioral therapy, drug therapy, and minimally invasive procedures.
Urinary incontinence (UI) in men facts
Multiple randomized controlled trials suggested worsening or no effect of estrogen upon urinary incontinence ( 31 , 32 ). However, estrogen cream was recommended in a 1996 guideline for incontinence treatment ( 33 ) and is increasingly used for vaginal symptoms since the women’s health initiative discouraged routine oral estrogen use ( 34 ).
It is as if their bladders were constantly overflowing, hence the general name overflow incontinence. Mixed incontinence is not uncommon in the elderly female population and can sometimes be complicated by urinary retention, which makes it a treatment challenge requiring staged multimodal treatment.
Women often abstain from daily activities that may cause urine leakage and many women stop exercising resulting in depression. How to overcome stress urinary incontinence (sui)?.
What causes urinary incontinence (UI) in men?
For urge ui, options include botulinum toxin a injections, percutaneous sacral nerve stimulation, augmentation cystoplasty (whereby a detubularised segment of bowel is inserted into the bladder wall to increase bladder capacity), or urinary diversion via ileal conduit.
Urinary incontinence (involuntary loss of urine) is twice as common in women as in men and affects at least 1 in 3 older women.
For example, in that 2008 study, 6. 5% of women who had never given birth reported urinary incontinence, whereas 23.
How is urinary incontinence (UI) in men diagnosed?
This review summarizes the evaluation and therapeutic options for women affected by urinary incontinence. The initial assessment should focus on understanding the effect of incontinence on quality of life, the patient's goals and preferences for treatment, the results of previous treatments, and the presence of concomitant conditions, such as advanced pelvic organ prolapse, that may require referral.
Urinary incontinence (ui) is a common condition in men and women that involves the involuntary loss of urine. It can occur while laughing, coughing, sneezing or jogging, which is known as stress incontinence.
Healthier lifestyle: if you were training and exercising before being diagnosed with urinary incontinence, you won't have to stop. With the best incontinence products for men and women, you are able to live an active life which keeps health problems such as high blood pressure, heart problems and other at bay.
How is urinary incontinence (UI) in men treated?
The purpose of this joint document of the american college of obstetricians and gynecologists and the american urogynecologic society is to review information on the current understanding of urinary incontinence in women and to outline guidelines for diagnosis and management that are consistent with the best available scientific evidence.
Stress urinary incontinence (sui) is a leakage of urine during moments of physical activity that increases abdominal pressure, such as coughing, sneezing, laughing, or exercise.
This process is highly beneficial in stress incontinence. In men, an artificial urinary sphincter is inserted. This is a small device, filled with fluid, and is placed around the bladder neck to help keep the sphincter stay closed until the person is ready to urinate.
What medications relieve pain and treat urinary incontinence in men?
Urinalysis should be ordered for all patients. A step-wise approach to treatment is directed at the urinary incontinence subtype, starting with conservative management, escalating to physical devices and medications, and ultimately referring for surgical intervention.
Other medications such as diuretics , muscle. Behavior modification therapy. Behavior modification is a psychological approach to the treatment of urinary incontinence in which patients gradually increase the length of the time interval between voidings and "retrain" the bladder in other ways.
Treatment of urinary incontinence and other related problems. Treat problems related to menstruation like excessive bleeding, pain, and endometriosis. Laparoscopic procedure to treat internal problems, including tumors.
Resources for urinary incontinence in men
”. Do these comments sound familiar? current estimates suggest that roughly 15 million americans experience urinary incontinence — the involuntary loss of urine — and that up to 85% of those affected are women.
The who noted that fgm could lead to “bleeding and infection, urinary incontinence, difficulties with childbirth and even death. ” the organization estimates that 130 million girls have undergone the procedure globally and 2 million are at risk each year, despite international agreements banning the practice.
There are several triggers, types and causes – with most cases occurring in elderly, postmenopausal, parous women. In this article, we shall look at the classification, clinical features and management of urinary incontinence.
Top Urinary Incontinence Related Articles
One of the newest procedures used to eliminate urinary incontinence is btl emsella. This article will guide you through various topics related to btl emsella.
Know Your Risk Factor for Urinary Incontinence
Urinary incontinence surgery is more invasive and has a higher risk of complications than do many other therapies, but it can also provide a long-term solution in severe cases.
Many factors lead to incontinence. Risk factors & complications. Age and gender are not the only factors that lead to urinary incontinence, including: obesity, pregnancy, nerve injuries and more.
Health tip: identifying common bladder problems in women. Botox beats implant for urinary incontinence in women. Urinary incontinence risk rises slightly after vaginal birth, study finds.
What Causes Urinary Incontinence?
Neural pathways and urinary tract mechanisms that maintain continence may be normal. Mixed incontinence is any combination of the above types.
Many people with ms experience a range of bladder problems , including urinary incontinence. Urinary incontinence may range from occasional leaks when coughing or sneezing to sudden urges to urinate throughout the day, sometimes leaking before making it to the bathroom.
Myrbetriq (mirabegron) relaxes the muscles of the urinary bladder, reducing bladder spasms. Myrbetriq is used to treat the symptoms of overactive bladder, such as frequent or urgent urination and urinary incontinence.
What Are the Treatments for Urinary Incontinence?
Urinary incontinence happens when pee leaks from your bladder in between bathroom trips. A number of treatments are available. Yours will depend on what’s causing the problem and how serious it is.
If you’ve been experiencing urinary incontinence, advanced gynecology is here for you. Treatment of urinary incontinence may include behavioral or non-pharmacological treatments, medication, surgery, biofeedback, catheterization, or a combination of these approaches.
The treatment options for urinary incontinence depends on the severity of the condition. The doctor may first ask you to undergo self-care treatments.
Types of Urinary Incontinence & Their Treatment
There are four main types of incontinence:. The most common types of urinary incontinence in women are stress urinary incontinence and urge urinary incontinence.
Other therapeutic options may be available for your pet with usmi. Please consult with your veterinarian. Other types of urinary incontinence can occur; if you are concerned about your pets urinary habits, please consult with your veterinarian or feel free to contact the teaching hospital at: 530-752-1393.
This deficiency of estrogen can be a potential cause of oab. To properly understand the causes of oab, you will first have to be accustomed with the types of urinary incontinence.
Living With Urinary Incontinence? Don't Let It Be Your Secret
If symptoms of urinary incontinence are bothersome, interfere with activities of daily living, or cause people to curtail their social activities, people should see a doctor.
Venice, fl-dec. 16--urinary incontinence is one of the major problems today for millions of women. The condition is embarrassing enough to drive women to try secret, even dangerous, remedies that may or may not help.
- urinary tract infections. Urinary incontinence products. In addition to medication and exercises, living with incontinence involves the use of incontinence products that help the patients stay dry.
Urinary Incontinence - Types And Causes And Products
Two common types of urinary incontinence include:. Stress incontinence. Loss of urine when coughing, laughing or sneezing, or when walking, running, lifting heavy objects or exercising.
There are two main types of urinary incontinence:. Stress urinary incontinence the loss of urine with physical activity, coughing or sneezing.
1. Know your supplies:. There are many types of adult diapers and incontinence pads available in the market today. When purchasing, make a checklist of what to look for in a product, such as the level of absorbency , odour control, the type of products needed (pull-up/tape on) and efficiency of changing the product.
3.6.1.5 Urinary Incontinence
The first thing i thought of when i read your question was hormone induced urinary incontinence. This would explain why she seems more bloated in the morning.
Neurourol urodyn 2015; 34: 128-132. 5. Resnick nm. Urinary incontinence in the elderly. Medical grand rounds 1984; 3: 281-290. 6. Newman d.
Practicing yoga asanas like the malasana (garland pose) and utkatasana (chair pose) also help strengthen your pelvic muscles. Urinary incontinence or the loss of ability to hold in the urine in your body can be embarrassing and inconvenient, interfering with your daily life.
What types of urinary incontinence exist?
The two most common types of urinary incontinence include stress urinary incontinence and overactive bladder syndrome (oab), or mixed urinary incontinence which is a combination of both.
Members of the neurology and urinary incontinence programs at upmc are world leaders in the exploration of new and innovative therapies for all types of urinary incontinence.
But how do you treat incontinence? to start with you need to find out which type you suffer from. There are several types of urinary incontinence, including the following:.
Find Urinary Incontinence Care Near You
The two main types of incontinence in women, stress urinary incontinence and urge urinary incontinence, can be evaluated by history and simple clinical assessment available to most primary care physicians.
Urinary incontinence is a socially devastating condition. The solution lies in finding the perfect adult diapers for men thus gaining confidence and being able to deal efficiently with the embarrassment or social isolation that is associated with incontinence.
Loyola provides truly integrated clinical care for urinary incontinence, bringing together specialists in urology , urogynecology , gynecologic surgery and reconstructive pelvic surgery to provide women with advanced care in a compassionate environment.
Relieve Yourself of Urinary Incontinence in Des Moines
Des moines is some to some highly qualified urologists. Find a highly professional urologist. If you are suffering from urinary incontinence in des moines, find a doctor that specializes in your area of need.
A good doctor keeps track of your progress and results of the treatments. Professional treatment of urinary incontinence in des moines ensures that you don’t sit back and let life happen to you.
Transient Urinary Incontinence
Dowling-castronovo, a. (1985). Urinary incontinence assessment in. Older adults part i - transient urinary incontinence. Obstetrics and. Gynecology, 109(2), 277-280.
Urgency urinary incontinence, mixed urinary incontinence, overflow. Urinary incontinence, transient urinary incontinence, functional urinary. Incontinence, older adults. Doi: 10. 7257/1053-816x. 2015.
Chronic Urinary Incontinence
This is the most common type of urinary incontinence in women. A chronic cough from smoking can make stress incontinence worse.
Overflow incontinence, also called chronic urinary retention, is often caused by a blockage or obstruction affecting your bladder. Your bladder may fill up as usual, but because of an obstruction, you will not be able to empty it completely, even when you try.
The u of m study found that this is not the case. Those conditions, such as constipation, diabetes, obesity, chronic lung disease and depression were found to be the same in both races and cause urinary incontinence to occur at comparable rates between the two.


